Traditionally, head and neck cancers are associated with risk factors like smoking and alcohol use. Rates of these smoking-related oral cancers are dropping, but the number of HPV related oral cancers are dramatically on the rise.
Nearly 90 per cent of adults have been infected with HPV and while most people clear the virus, it can linger in some and become cancerous over decades
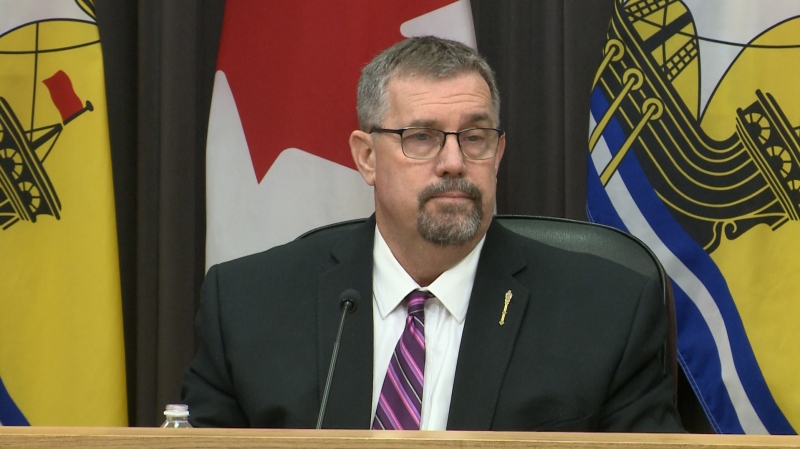
As a head and neck surgeon at the QEII Health Sciences Centre, Dr. Matthew Rigby has seen the rise of HPV related oral cancers first hand.
Dr. Rigby says most of these types of cancers he treats are in the oropharynx, affecting the tonsils and the base of the tongue. It's an area that can be hard for surgeons to reach.
“Traditionally we did that by cutting the jaw bone and swinging it over and actually getting to the back of the throat,” says Rigby.
Now, Rigby is one of a handful of surgeons in the country who treats these cancers using laser microsurgery.
“So it's basically a metal scope that allows me to see the cancer straight on and then we bring a microscope in and use laser to cut the tumour out in parts. That gives me access to the tumour and I can cut it out without major surgery just to get there,” says Rigby.
Recovery time is typically much faster than traditional surgery and Dr. Rigby says patients also tend to function better afterward.
“They swallow better, their voice is better, almost always they'll need a breathing tube if they have their jaw split. They hardly ever need a breathing tube or tracheostomy if they have the tumour removed through their mouth,” says Rigby.
Halifax is the only centre in Canada to offer this treatment. It's also the home of research around this growing health concern.
Dr. Rob Hart is a head and neck surgeon. He is trying to better understand why HPV develops into cancer in some cases.
“There's been about a 225 per cent increase in oropharynx cancer caused by HPV over the past decade,” says Hart. “Many people are infected with HPV, probably 100% of us have contacted it at some point in our lives, but what percentage of those people develop a cancer and why is the real question.”
Researcher Dr. Jim Fawcett says this kind of work could help identify bio-markers for HPV and eventually lead to tests in a clinical setting.
“What we're doing is trying to understand what are those cellular mechanisms, what is the HPV virus making, and who are those viral proteins talking to in the cell to disrupt and start the process of cancer in the cells,” says Fawcett. “When you come into the clinic, we want to be able to use this kind of research to say you know, you've got these kinds of markers, these kind of things are happening, and we know if that happens that's bad versus this one.”
Dr. Hart says their end goal is to prevent HPV from causing cancer.
“We're a long way from that. If we can't do that, then the next step would be really to develop therapeutics, so chemotherapies based on this model that would significantly change the outcome in those patients,” says Hart.