N.S. family doctor of 43 years says the province's doctor shortage is not surprising
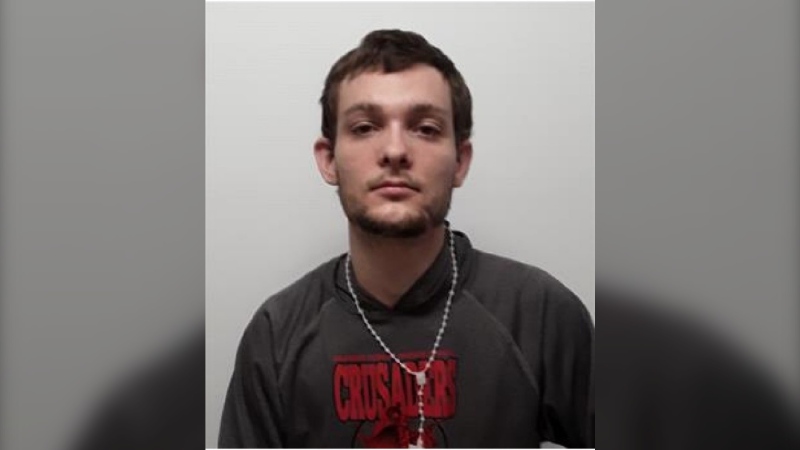
 Dr. George Burden, who has been a physician in Nova Scotia for 43 years, has announced his retirement. (Dr. George Burden/Facebook)
Dr. George Burden, who has been a physician in Nova Scotia for 43 years, has announced his retirement. (Dr. George Burden/Facebook)
A Nova Scotia doctor of 43 years says the province's shortage of family doctors is an issue decades in the making -- made more acute by an aging population.
Dr. George Burden was "at the tender age of 23" when he fell in love with family medicine, but he says he's not surprised that the province is struggling to find enough primary care doctors.
"Family practice is the best, you get to build such good relationships when you're in an area for some time," he said in a recent interview. "People almost consider you part of the family."
The dynamics of family medicine have changed significantly over his career because of the rise in the average age of patients, Burden said.
"Back 40 years ago, about one patient in 20 was over 65, so my patient encounters were quicker with far less paperwork," Burden said. "As people get older, there are much more complex things going on."
According to a 2021 Statistics Canada report, there are nearly 216,000 Nova Scotians 65 and older, representing more than 21 per cent of the population.
"This group takes up most of my time, leaving little availability for acute issues, which often end up in the ER, clogging up (ER doctors') ability to deal with more serious emergencies," he said.
Burden cares for about 2,000 patients in Elmsdale, a village in central Nova Scotia, where he's been practising for his entire career. Late last month, Burden was struck by a car at a crosswalk, which he said gave him "a wake-up call" and pushed him toward retirement.
"I was lying on the ground looking up from the underside of the car, with a tire about a foot from my head, and I kind of had a revelation," he said, adding that he hopes to spend more time with family and his grandson overseas.
He also suffered injuries to his wrist and thumb in the accident, which he said made work more challenging and contributed to his decision to retire this winter.
Burden says he'll retire at the end of January, and he has told his patients to join the province's Need a Family Practice registry, where more than 105,000 Nova Scotians were registered as needing a primary care physician as of Aug. 1.
The doctor said Nova Scotia's current shortage of physicians can be traced back to the 1991 national Barer-Stoddart report, which was commissioned by the federal government. The report said there were too many doctors graduating from medical school in Canada and it recommended reducing enrolment and lowering the ratio of physicians to patients.
"A lot of governments grabbed onto it as an excuse to basically get rid of a lot of doctors, which they did by cutting medical school enrolments, which usually shows its effect about 10 years later," Burden said.
Around the same time the Barer-Stoddart report came out, Nova Scotia froze physician fees, Burden said, which "meant about a 30 per cent cut in pay all of a sudden." That decision led to many of Burden's colleagues leaving the province, he said, adding that some went to the United States and to other provinces.
Burden doesn't have anyone ready to take over his practice, though not for lack of trying. In 2020, Burden said, he began mentoring a doctor who was working on certifying her international medical training to practise in Nova Scotia. He had hoped to work with her for a year or so before she took over his patients.
"But she is still no closer to getting approval two years later," he said.
Burden said he would like to see the province speed up the process for doctor licensing and certification in Nova Scotia.
But he is encouraged by the province's progress in supporting collaborative-care clinics like his and by the new rural doctor medical school seats Nova Scotia announced in May. That program established five new medical school seats for students who will agree to work in a rural family practice for five years after graduation.
"You'll get them in with the community, and it'll happen with them as it happened with me, which is they'll fall in love with the community and maybe they'll keep the practice going," he said.
"There's not anything that I would have traded it for because of the wonderful relationship I've had with my patients over the years."
This report by The Canadian Press was first published Aug. 23, 2022.
This story was produced with the financial assistance of the Meta and Canadian Press News Fellowship.
CTVNews.ca Top Stories

'One of the single most terrifying things ever': Ontario couple among passengers on sinking tour boat in Dominican Republic
A Toronto couple are speaking out about their 'extremely dangerous' experience on board a sinking tour boat in the Dominican Republic last week.
Half of Canadians have negative opinion of latest Liberal budget: poll
A new poll suggests the Liberals have not won over voters with their latest budget, though there is broad support for their plan to build millions of homes.
opinion Why you should protect your investments by naming a trusted contact person
Appointing a trusted person to help with financial obligations can give you peace of mind. In his personal finance column for CTVNews.ca, Christopher Liew outlines the key benefits of naming a confidant to take over your financial responsibilities, if the need ever arises.
Teacher shortages see some Ontario high school students awarded perfect grades on midterm exams
Students at a high school in York Region have been awarded perfect marks on their midterm exams in three subjects – not because of their academic performances however, but because they had no teacher.
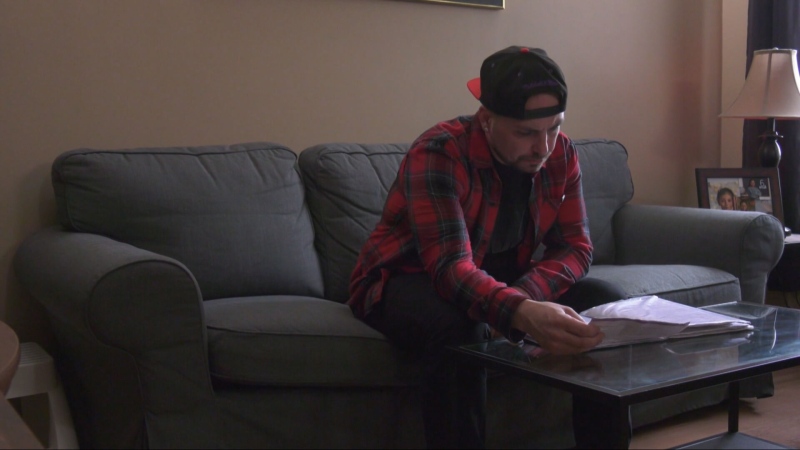
'My stomach dropped': Winnipeg man speaks out after being criminally harassed following single online date
A Winnipeg man said a single date gone wrong led to years of criminal harassment, false arrests, stress and depression.
Doctors combine a pig kidney transplant and a heart device in a bid to extend woman's life
Doctors have transplanted a pig kidney into a New Jersey woman who was near death, part of a dramatic pair of surgeries that also stabilized her failing heart.
Photographer alleges he was forced to watch Megan Thee Stallion have sex and was unfairly fired
A photographer who worked for Megan Thee Stallion said in a lawsuit filed Tuesday that he was forced to watch her have sex, was unfairly fired soon after and was abused as her employee.
Ottawa injects another $36M into vaccine injury compensation fund
The federal government has added $36.4 million to a program designed to support people who have been seriously injured or killed by vaccines since the end of 2020.
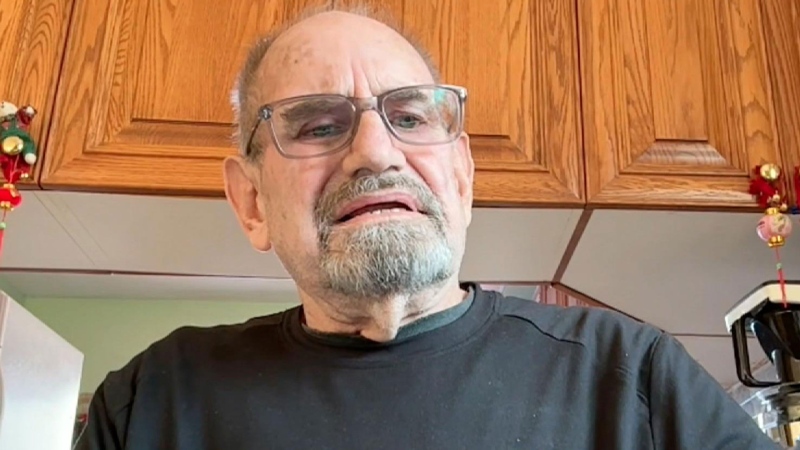
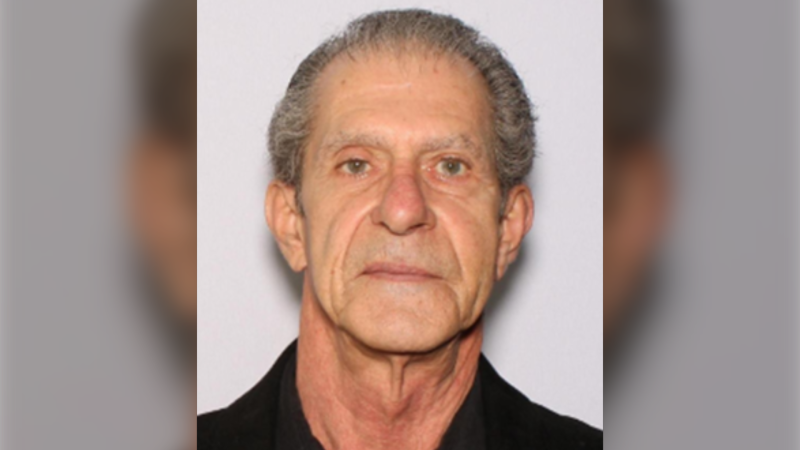
An Ontario senior thought he called Geek Squad for help with his printer. Instead, he got scammed out of $25,000
An Ontario senior’s attempt to get technical help online led him into a spoofing scam where he lost $25,000. Now, he’s sharing his story to warn others.