Nurse practitioner-led clinics would help alleviate pressure on Maritime ERs: professor and NP
Following Nova Scotia's announcement of extra resources to help alleviate the pressure on strained emergency departments, nurses throughout the province have been sharing their thoughts on the new plan.
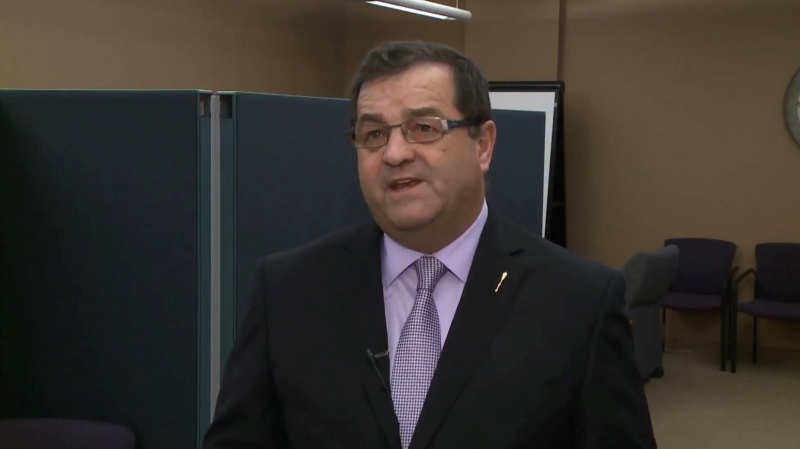
Tammy O'Rourke is an online associate professor with Athabasca University in Athabasca, Alta., and a nurse practitioner (NP) who recently moved to Cape Breton.
With more than 30 years in acute and primary care, and older adult and women's health, O’Rourke has created, developed and established two nurse practitioner-led clinics -- one in Edmonton and another in Ontario.
She says an NP-led clinic has three distinct characteristics.
"One, it has a board of directors that is represented 50 per cent by nurse practitioners who don't work at the clinic. The clinical lead is a nurse practitioner, so he or she makes the decisions about the type of care that will be received and how the funding will be spent on what services. And the most responsible provider for the patient is the nurse practitioner," she said during an interview with CTV Atlantic on Thursday.
"They work quite autonomously within those models to manage their own panel of patients, which can be anywhere from 800 to 1,000. As we know, one patient isn't the same as all patients, so sometimes having a panel of 600 can be quite heavy if they're older with chronic disease. And patients really like the model."
O’Rourke feels a lot of patients still don't know what a nurse practitioner is and how they function.
As far as what types of ailments an NP-led clinic can treat, O’Rourke says they can help with anything a family physician could treat.
"So, it would look exactly the same to the front-facing user. It's just that the label on my profession is different than the label on the medical profession," she said. "So, as a nurse practitioner, I write prescriptions for everything, I diagnose, I order MRIs, CT scans, ultrasounds, everything that you would need."
During the summer of 2022, O’Rourke moved to Cape Breton, giving her some time to assess Nova Scotia's health-care situation.
She believes a NP-led clinic would work in Nova Scotia and in the Maritimes in general.
"Absolutely. And we see them work very well in Ontario. There's 25 now that are still open. The one that I opened in Ontario is now, I think, 11 years into operation and we have NPs, registered nurses, practical nurses, pharmacists. We even had a chiropractor at that clinic," said O’Rourke.
"And the one in Edmonton was senior-focused, so we specifically developed services from a senior’s perspective. We interviewed them to see what they wanted in their primary care and we put that into the clinic and I believe that would go very well. Especially because my husband said to me, 'Are you going to open a clinic in Cape Breton?' And I said, 'Oh, I don't know. That's a lot of work.'"
According to O’Rourke, in the United States, the ratio for NP staffing is 40 NPs to 100,000 people. She says in Canada, that ratio currently sits at four NPs to 100,000 people.
She says similar data hasn't been released for Nova Scotia specifically.
"So, our ratio is really low here [Canada]. We have lots of room to increase and improve. Athabasca University is the largest educator of NPs and we've educated at least one-third of NPs in Canada," said O’Rourke.
O’Rourke listened to Nova Scotia's recent announcement on how it plans to better serve residents at emergency departments in a more timely fashion.
Earlier this week, officials outlined extra measures to improve ambulance response times, address long wait times and overcrowding in Nova Scotia’s ERs, and offer people more places to receive care.
She believes the plan is "a bit vague."
"I believe that the public has the right to know the exact numbers. Like how much of a deficit are we in in Nova Scotia? What are our targets over the next three, six, nine, 12 months? Because these solutions don't come easy and the annual accountability report of emergency departments that looked at April 2021 to March 2022, they introduced some of the same ideas, but those haven't been put into place yet," said O’Rourke.
O’Rourke says she too has had her own experience with a Nova Scotia emergency department after her son injured himself at a beach in Ingonish, N.S.
"He sprained his ankle. Well, his ankle blew right up and he couldn't walk on it. So, the fact that he couldn't walk on it, I said well I better go get an X-ray. So, I went to the emergency room and I was waiting for 12 hours and I thought, 'Oh, jeepers. This is a long time.' So then I said, I'm going to sit here, I'm just going to have this experience and see what it's like in the emergency room in Cape Breton. And I sat there for 18 hours waiting for an X-ray that a NP could have given me in five minutes," she said.
"They could have done a quick assessment, ordered the X-ray, saw that it wasn't a break and sent me out the door with a wrap and instructions on rest, compression and elevation, but that wasn't the experience. I had to wait 18 hours in an emergency room filled with people, no access to food, and most of the patients, I could hear them talking about what they were there for, and I'm thinking, 'A NP could clear probably 50 to 75 per cent of this room."
CTVNews.ca Top Stories

Young people 'tortured' if stolen vehicle operations fail, Montreal police tell MPs
One day after a Montreal police officer fired gunshots at a suspect in a stolen vehicle, senior officers were telling parliamentarians that organized crime groups are recruiting people as young as 15 in the city to steal cars so that they can be shipped overseas.
Mandisa, Grammy award-winning 'American Idol' alum, dead at 47
Soulful gospel artist Mandisa, a Grammy-winning singer who got her start as a contestant on 'American Idol' in 2006, has died, according to a statement on her verified social media. She was 47.
Man sets self on fire outside New York court where Trump trial underway
A man set himself on fire on Friday outside the New York courthouse where Donald Trump's historic hush-money trial was taking place as jury selection wrapped up, but officials said he did not appear to have been targeting Trump.
Sask. father found guilty of withholding daughter to prevent her from getting COVID-19 vaccine
Michael Gordon Jackson, a Saskatchewan man accused of abducting his daughter to prevent her from getting a COVID-19 vaccine, has been found guilty for contravention of a custody order.
She set out to find a husband in a year. Then she matched with a guy on a dating app on the other side of the world
Scottish comedian Samantha Hannah was working on a comedy show about finding a husband when Toby Hunter came into her life. What happened next surprised them both.
Shivering for health: The myths and truths of ice baths explained
In a climate of social media-endorsed wellness rituals, plunging into cold water has promised to aid muscle recovery, enhance mental health and support immune system function. But the evidence of such benefits sits on thin ice, according to researchers.
'It could be catastrophic': Woman says natural supplement contained hidden painkiller drug
A Manitoba woman thought she found a miracle natural supplement, but said a hidden ingredient wreaked havoc on her health.
'It was joy': Trapped B.C. orca calf eats seal meat, putting rescue on hold
A rescue operation for an orca calf trapped in a remote tidal lagoon off Vancouver Island has been put on hold after it started eating seal meat thrown in the water for what is believed to be the first time.
Manitoba mom praises quick-thinking fire department for freeing daughter stuck in playground equipment
A Manitoba mother is praising firefighters for their quick work in helping her daughter who got stuck at a playground in Lorette, Man.